Brain Fog
Is "brain fog" or issues with attention/concentration a real physical symptom of POTS? If so, what can be done about it?
Dr. Schofield: “Brain fog” or cognitive dysfunction is a common symptom in many chronic diseases, including celiac disease, lupus, multiple sclerosis and mast cell disease. It is also almost universal in patients with POTS—reported by >95%—and most experience this symptom on a daily basis! It ranges in severity from mild to very severe. Brain fog means there is a significant enough problem with one’s thinking to interfere with daily functioning.
The precise mechanism by which brain fog occurs in POTS is incompletely understood, but its presence has been confirmed by formal neurocognitive testing in patients with autonomic disorders. Patients with POTS have been shown to have difficulty with attention, concentration, memory, executive function and processing speed. It has been shown that there are complex alterations in the regulation of brain blood flow and brain fog may be worse in the upright position in patients with POTS, but there are likely other mechanisms involved including inflammation from immune dysregulation, etc. as most POTS patients experience brain fog sitting and laying in addition to when standing. Furthermore, many patients with POTS notice cognitive issues as part of post exertional malaise. Just as overdoing physical exertion may result in a “crash” or flare, too much mental exertion can result in a similar escalation of symptoms.
The treatment of brain fog in patients with POTS is to treat the underlying autonomic dysfunction with salt and fluids, exercise and medications when deemed appropriate. If there is a known underlying cause for the patient’s POTS such as mast cell activation syndrome, it is usually helpful to treat that as well. For patients with severe autoimmune forms of POTS, treating the underlying autoimmunity (e.g. with IVIG or rituximab) may be required and in these patients cognitive dysfunction usually improves together with the other symptoms. Patients with POTS associated with antiphospholipid antibodies (aPL) may notice dramatic improvement in memory loss with medications that thin the blood, including aspirin, clopidogrel and/or anticoagulants, but these patients may have more than one mechanism contributing to their cognitive dysfunction and the blood thinning medications may only improve one aspect of the memory issues. In my experience, the memory loss associated with the “sticky blood” caused by antiphospholipid antibodies tends to be more severe than that seen in patients with POTS without aPL and it is not uncommon for these patients to be seriously concerned they may have a very early onset of Alzheimer’s disease!
Reference: Raj V, Opie M, Arnold AC. Cognitive and psychological issues in postural tachycardia syndrome. Auton Neurosci. 2018 Dec; 215:46-55.
Dr. Fedorowski: It all depends on what you want to call “a real physical” symptom. Rodriguez et al. (2019) state that “POTS patients show deficits in working memory exclusively in the upright position compared to healthy subjects” whereas Arnold et al. 2015 “provides evidence for deficits in selective attention and cognitive processing in patients with POTS.” In general, there are multiple reports on various types of cognitive impairment among patients with POTS but a definitive consensus is lacking.
However, as far as “real physical findings” are concerned, POTS patients demonstrate significant reduction of cerebral oxygenation on standing, as shown in a study by Kharraziha et al. (2019) (see figure below).
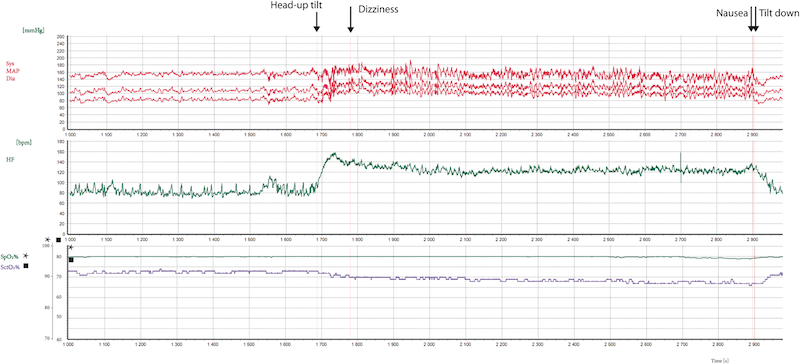
Example of a POTS patient during head-up tilt displaying changes in heart rate, blood pressure, and cerebral tissue oxygen saturation. Note the inverse correlation between heart rate and cerebral tissue oxygen saturation in this POTS patient during head-up tilt.
Thus, there is proof that cerebral circulation may be impaired on standing in POTS. The reason for it is not fully understood yet.