Testing for POTS
There are many different tests that practitioners can use to assess if a patient has POTS.
Tilt Table Test
The tilt table test is used by autonomic physicians as the gold standard test for POTS. In this procedure, the patient will be put on a table that can be adjusted from the horizontal position to nearly vertical. The table has a footrest and two safety straps to prevent falling if dizziness or fainting should occur during the upright portion of the test. It is important to lay flat for some time before they start the actual testing. During this time, they will attach a blood pressure cuff, oxygen sensor, and EKG sensors. This allows the physician to monitor blood pressure, oxygen, heart rate, and electrical activity of the heart during testing.
Steps of the tilt table test:
- Baseline readings will be taken for at least five minutes prior to moving to the vertical position.
- The table will be moved from horizontal to about 70 degrees. This part of the test generally lasts for 10 minutes. If POTS is present, symptoms will likely appear during this phase of testing. Some faint, while others sweat, have hot flashes and abdominal pain or nausea.
- If fainting occurs, the table will be returned to the horizontal position immediately.
- It is important to stay as still as possible when vertical. Try not to tighten the muscles of your legs or buttocks while upright.
- Upon completion of the upright portion of the test, the table will be returned to the horizontal position, and your physician will continue to monitor both heart rate and blood pressure for an additional 15-20 minutes.

Standing Test
1. Lay patient supine for 10 minutes. Take pulse and blood pressure while still supine.
2. Stand patient up still as possible for 2 minutes without leaning or moving. Take the pulse and blood pressure every two minutes while standing.
POTS can be diagnosed a couple of ways:
If the heart rate is greater than 120 beats per minute at any point while standing, POTS might be indicated.
Adults age > 19, an increase in heart rate of 30 beats per minute or more between laying and standing may indicate POTS.
Children and teens age <19, an increase in heart rate of of 40 beats per minute or more when standing, it may be POTS.
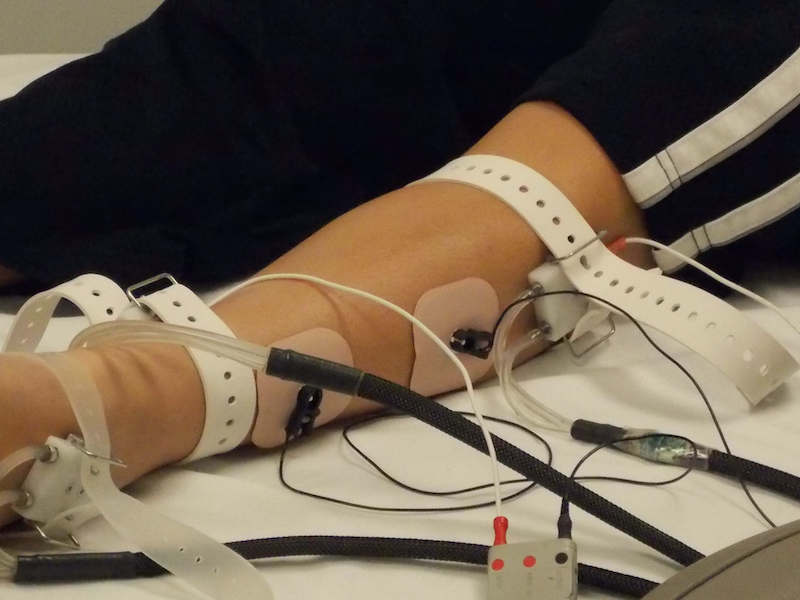
Quantitative Sudomotor Autonomic Reflex Testing (QSART)
This test measures the response of the small nerve fibers innervating the sweat glands. QSART can be used to assess disorders of the autonomic nervous system and peripheral neuropathies. There is a reservoir of the neurotransmitter acetylcholine which is released onto the skin with mild electrical stimulation. The QSART then measures the amount of sweat present.
If there is a loss of sympathetic neurons, sweat will not be detected during this test. This might indicate sympathetic cholinergic failure from loss of sympathetic nerves. It is possible for someone who doesn't sweat in hot and humid environments to sweat during the stimulation of the QSART test.
Steps of the QSART:
- The electrodes will be placed on three spots on the lower leg and one near the wrist. Shoes and socks will be removed. The skin will be wiped with acetone and then alcohol before the electrodes can be attached.
- The electrodes will be strapped to the arm and leg.
- The electrical stimulation will be turned on and the test will begin.
- The test takes approximately 45 minutes to complete.
Thermoregulatory Sweat Test
This is a measure of your ability to sweat when stimulated by a warm and humid environment. It assesses the autonomic control of sweating and body temperature regulation. In this test, an orange powder is applied to the skin and then the patient is put into a hot and humid environment that would cause perspiration in healthy individuals. The powder will change from orange to purple if sweating occurs. The pattern of sweating can help diagnose a variety of neurological and autonomic disorders related to reduced or excessive sweating such as small fiber neuropathy, autonomic neuropathy, multiple system atrophy, and pure autonomic failure among others.
Stress Test
The stress test can use a treadmill or a bike to determine how exercise affects a person with postural orthostatic tachycardia syndrome. You will exercise until you reach the target heart rate, typically 10-12 minutes. During this test, they measure both your heart via EKG and respiratory system using a respirometer.
Hand Grip Test
This is exactly what it sounds like – you squeeze a hand grip dynamometer. First, they measure your maximum grip strength. Then you squeeze to maintain a percentage of your maximum, often 30%, for a set period of time or until your arm is fatigued. Those with autonomic dysfunction may show an increase in their diastolic blood pressure as the sympathetic nervous system is activated during the hand grip test.
Valsalva Maneuver
The Valsalva Maneuver requires you to blow into a tube to maintain 40 mmHg for 15 seconds while your heart rate and blood pressure are being recorded. This may show abnormal baroreflex results in those with moderate to severe POTS. There is conflicting evidence on the accuracy of this particular test.
Heart Monitoring at Home
Sinus tachycardia is common in people with POTS. Wearing a Holter monitor, endless-loop recorder, or event recorder allows physicians to monitor your heart over days or weeks. You may be asked to keep a written journal of symptoms, or to push a button on the device when you faint or feel otherwise symptomatic. This highlights symptomatic episodes for a reading by your doctor.
Catecholamine Test: Blood or 24 Hour Urine Sample
Some people with postural orthostatic tachycardia syndrome will have abnormal function of their sympathetic nervous system. The major neurotransmitter of this system is norepinephrine, a catecholamine. Therefore, the catecholamine test can assess levels of sympathetic activity in a variety of situations. It is common to use an IV for blood draws to prevent distress at the time of the reading, as this would skew the results. Blood will be drawn after the patient has been horizontal for 20-30 minutes, and then again after being tilted to a standing position. In the case of the urine sample, it is an indicator of general levels of catecholamines, and does not give specific information about levels when standing versus sitting.
24 Hour Urinary Sodium Test
This can help to determine if your plasma volume is normal. Many with POTS struggle with low blood volume, and are treated with salt and excess hydration to restore normal blood volumes. Low sodium in the urine means that the body is retaining salt and water to try to increase blood volume.